Insights
We offer personalized insights and strategy, and spotlight data in a compelling way to shape policy, communicate value, secure reimbursement, and drive patient access.
-
How The 340B Program Impacts Federal & State Tax Liability
While the 340B drug pricing program is often touted as cost-free to taxpayers, our analysis estimates the tax impact of the program for both self- and fully insured employees and workers across the US.
-
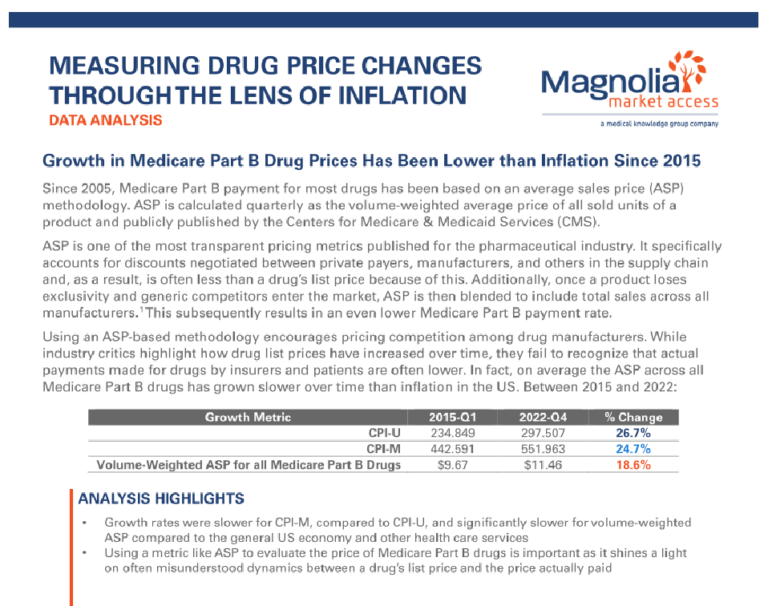
Measuring Drug Price Changes Through the Lens of Inflation
A data analysis comparing growth rates of US inflation and Medicare Part B drug prices (2015-2022) reveals that average sales price (ASP) has grown slower than inflation, making it a more transparent and relevant metric than list prices for evaluating medical spending trends.
-
Issue Brief: Federal-Level Policy Solution to Reduce Costs for 340B Patients
Magnolia Market Access analyzed a potential sliding fee scale policy, adjusting patient cost-sharing for 340B-dispensed drugs, to understand implications on out-of-pocket costs for 340B patients.
-
Issue Brief: State-Level Policy Solution to Reduce Costs for 340B Patients
Magnolia Market Access analyzed a potential sliding fee scale policy, adjusting patient cost-sharing for 340B-dispensed drugs, to understand implications on out-of-pocket costs for 340B patients.
-
Building a Comprehensive Go-To-Market Strategy Through Stakeholder Ecosystem Mapping
A mid-size client was preparing for a product launch and needed assistance facilitating a successful go-to-market strategy. The company sought to identify and understand the entire stakeholder landscape and create short- and long-term stakeholder engagement strategies to meet the needs of their entire organization.
-

Market Access Segmentation & Identification
A biopharma company engaged Magnolia Market Access and sister company, 81qd, to collect data and segment provider and payer entities to identify key decision makers for a novel cardiology treatment.
-
Using EMR Data to Support Budget Impact Modeling
A large pharmaceutical company needed to demonstrate the potential cost savings of placing a new drug on payer formularies.
-
Calculating Adherence in the Presence of Variable Follow-Up
A small-size pharmaceutical company was interested in using real-world evidence to compare adherence between two formulations of an oral oncology treatment for Multiple Myeloma (MM).
-
Using Real-world Data to Support Product Label Change
A mid-size pharmaceutical company was interested in obtaining real-world evidence demonstrating the safety and effectiveness of higher dosage chemotherapy for a labeled oncology indication.
-
MMA IRA Payer Insights Survey
Magnolia Market Access has just released its fourth IRA Payer Insights Survey. This chartbook provides an overview of findings from the 34 payers and actuaries surveyed and interviewed regarding the future Medicare Drug Price Netoriation Program, Part D Redesign, and the Medicare Prescription Payment Program.
-
Objection Handling: How Should Manufacturers Evolve to Meet the Clinical and Contracting Demands of Payers?
Navigating Market Access with Magnolia Summer 2024 Presentation.
-
Identifying the Market, Business and Reimbursement Potential for Cell Therapies
Magnolia was asked to assess which type of cell therapies and disease states offered the greatest potential for development, and also wanted to further understand the benefits of creating an autologous or allogeneic product.