Prescription Drug Affordability Boards: Considerations to Ensure Patient Access
State Strategies for PDAB Implementation:
Analyzing the PORTAL Toolkit
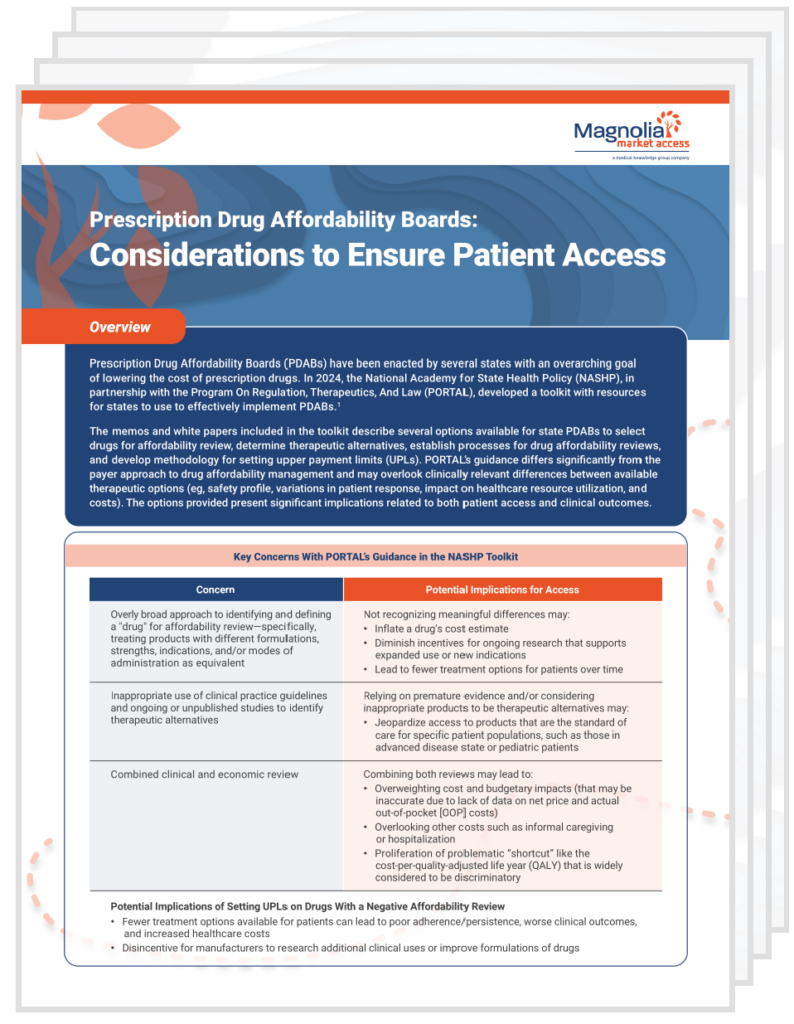
Prescription Drug Affordability Boards (PDABs) have been enacted by several states with an overarching goal of lowering the cost of prescription drugs. This issue brief discusses concerns with and the potential implications of a resource toolkit (developed by the National Academy for State Health Policy [NASHP], in partnership with the Program On Regulation, Therapeutics, and Law [PORTAL]) to assist states with effectively implementing PDABs.
Key insights include:
- Drug selection for affordability review: Overly broad drug aggregation can result in not recognizing meaningful differences of various product formulations and strengths that are developed to address specific patient needs to achieve identified therapeutic goals.
- Therapeutic alternative determination: Relying primarily on clinical practice guidelines and ongoing or unpublished clinical trials, rather than defining therapeutic alternatives based on FDA approval in matched indications and populations and actively engaging clinical experts to validate, can lead to an unfavorable affordability decision based on clinically inaccurate comparisons.
- Affordability reviews and setting upper payment limits (UPLs): Combining the clinical and economic review may undervalue the clinical benefit of a product and introduce bias by primarily focusing on cost and budgetary impacts that are not accurate due to lack of data on net price and actual patient out-of-pocket costs.
Download the issue brief to learn more about how implementation of the PORTAL guidance without flexibility in those states with the authority to set UPLs could lead to decreased patient access to the therapeutic options chosen by the patient and prescriber, and possibly to all therapeutic options.